Acute Pain and Activity Intolerance - NCP Angina Pectoris
Nursing Diagnosis Care Plan Angina Pectoris
Angina pectoris is the result of myocardial ischemia caused by an imbalance between myocardial blood supply and oxygen demand.
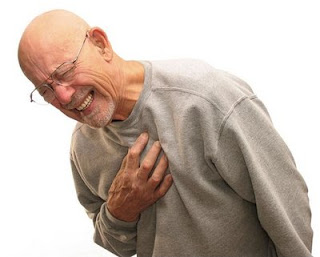
Angina, or angina pectoris, is the medical term used to describe the temporary chest discomfort that occurs when the heart is not getting enough blood.
Not all chest pain is angina. Pain in the chest can come from a number of causes, which range from not serious to very serious.
For example, chest pain can be caused by:
- acid reflux (gastroesophageal reflux disease, GERD),
- upper respiratory infection,
- asthma, or
- sore muscles and ligaments in the chest (chest wall pain)
Go to a hospital emergency department if the patient has any of the following with chest pain:
- Other symptoms such as: sweating, weakness, faintness, numbness or tingling, or nausea
- Pain that does not go away after a few minutes
- Pain that is of concern in any way
Acute Pain Nanda Definition : Unpleasant sensory and emotional experience arising from actual or potential tissue damage or described in terms of such damage (International Association for the Study of Pain); sudden or slow onset of any intensity from mild to severe with an anticipated or predictable end and a duration of less than 6 months
Activity Intolerance Nanda Definition : Insufficient physiological or psychological energy to endure or complete required or desired daily activities.
Nursing Diagnosis and Interventions for Angina Pectoris
1. Acute Pain related to myocardial ischemic
Intervention :
- Assess the factors that aggravate the pain.
- Create a calm environment, limit the visitor when necessary.
- Give soft foods and let the client rest 1 hour after meals.
- Stay with clients who are experiencing pain or anxious.
- Put the client on bed rest during episodes of angina (the first 24-30 hours) with a semi-Fowler position.
- Observation of vital signs every 5 minutes every attack of angina.
- Teach distraction and relaxation techniques.
- Collaboration treatment.
2. Activity intolerance related to decreased cardiac output
Intervention :
- Increase client activity on a regular basis.
- ECG Monitor with frequently.
- Maintain bed rest in a comfortable position.
- Provide adequate rest periods, aids in the fulfillment of self-care activities as indicated.
- Note skin color and pulse quality.